Head trauma-brain trauma
The most feared consequence of a head trauma is brain injury.Mechanisms of brain injury :
Primary injury: This is the initial injury and it is mechanically induced: Direct contact (eg, an object striking the head ) and acceleration-deceleration causing the brain to move inside the skull.
Secondary injury is brain damage not mechanically induced, it may be delayed from the moment of the head trauma and can be due to brain edema, a developing intracranial hematoma, increased intracranial pressure, decreased brain (cerebral) perfusion pressure (ischemia of the brain).
Cerebral perfusion pressure (CPP), intracranial pressure and the Monro-Kellie hypothesis.
Decreased cerebral perfusion pressure (CPP) can result from reduced mean arterial pressure (MAP) or from increased intracranial pressure (ICP). Increased ICP in trauma can be due to cerebral edema, or an intracranial hematoma. This knowledge stems from the equation CPP = MAP - ICP. The brain receives approximately 15% of cardiac output.The Monro–Kellie hypothesis states that since the skull is a rigid bony stucture, the sum of the volume of the brain, blood, and cerebrospinal fluid within the skull remains constant. Therefore, an increase in the volume of one of the above intracranial contents (eg increased volume of blood due to an intracranial hematoma) must be offset by a decreased volume of the others and will soon result in an increased intracranial pressure (ICP). A severely increased ICP can thus result in cerebral herniation, or when ICP approximates the systolic blood pressure, cerebral blood flow ceases and this causes brain death.
Cervical spine protection
It is important to suspect every patient with blunt injury to the head of having cervical spine injury until proven otherwise ( Cervical spine injury occurs overall in about 5% of all blunt head injuries and the greater the force, the greater the risk of cervical spine injury). Immobilize the cervical spine during evaluation of the patient by manual stabilization and during transport with an appropriately sized and fitted cervical collar.In a patient with severe head injury full spinal immobilization is usually needed before transfer to the hospital
Airway and breathing
Hypoxia is associated with increased morbidity and mortality in trauma patients and especially in patients with traumatic brain injury. Thus, hypoxia should be avoided or corrected promptly. Allpatients with head injury should initially receive 100% oxygen by high-flow mask.
The airway must be kept open and clear. Suctioning of blood and secretions and removal of foreign bodies and dental appliances is necessary in many cases.Indications to secure the airway with endotracheal intubation are: Loss of gag reflex, inability to adequately clear secretions, or Glasgow Coma Scale (GCS) score ≤ 8.
During endotracheal intubation in a patient with head trauma manual cervical immobilization must be maintained. Apneic or hypoventilating patients should be ventilated with an
Ambu bag and mask and 100% oxygen until intubation can be accomplished. Avoid overventilation because this causes hypocarbia (lower concentration of carbon dioxide in blood) and this can lead to cerebral vasospasm.
AMPLE:
A- Allergies
M- Medications (especially anticoagulants)
P- Past medical history
L- Last meal (the time of last meal)
E- Events related to the injury : Mechanism and circumstances of injury, was there loss of consciousness and for how long ? Does the patient have nausea, vomiting, visual difficulty or impairment, headache (mild, moderate or severe) ?
Seek for evidence of external trauma (a laceration, ecchymosis, etc) Scalp trauma can cause significant hemorrhage, because it is a highly vascular area. Seek for evidence of skull fracture (eg a depressed scull injury) and especially for signs indicating a basilar skull fracture, such as periorbital ecchymosis, ecchymosis behind the ear (Battle sign), cerebrospinal fluid ottorrhea or rinorrhea (a clear fluid running from the ears or nose), hemotympanum ( blood behind ear drum: the presence of blood in the tympanic cavity of the middle ear, diagnosed by otoscopy, presenting as partial or total occupancy of the tympanic membrane by a bright red to black-blue color depending on the duration of the blood in tympanic cavity).
Neurological examination:
Glascow coma scale (GSC)
During endotracheal intubation in a patient with head trauma manual cervical immobilization must be maintained. Apneic or hypoventilating patients should be ventilated with an
Ambu bag and mask and 100% oxygen until intubation can be accomplished. Avoid overventilation because this causes hypocarbia (lower concentration of carbon dioxide in blood) and this can lead to cerebral vasospasm.
History obtained in case of head trauma
Information obtained from family members and bystanders is very useful in many cases.AMPLE:
A- Allergies
M- Medications (especially anticoagulants)
P- Past medical history
L- Last meal (the time of last meal)
E- Events related to the injury : Mechanism and circumstances of injury, was there loss of consciousness and for how long ? Does the patient have nausea, vomiting, visual difficulty or impairment, headache (mild, moderate or severe) ?
Physical examination of the patient with head /brain injury
Rapid assessment of the ABCs (airway, breathing, circulation), as in any trauma patient. Assessment of the depth and rate of respirations, pulse rate and the blood pressure is essential. The presence of hypertension and bradycardia in the setting of head trauma should raise the suspicion of severely increased intracranial pressure. This finding is called the Cushing reflex and it is a reaction that tends to maintain the cerebral perfusion pressure. Hypotension usually is not caused by head injury, thus in such a case be careful to search for other injuries causing external or internal hemorrhage.Seek for evidence of external trauma (a laceration, ecchymosis, etc) Scalp trauma can cause significant hemorrhage, because it is a highly vascular area. Seek for evidence of skull fracture (eg a depressed scull injury) and especially for signs indicating a basilar skull fracture, such as periorbital ecchymosis, ecchymosis behind the ear (Battle sign), cerebrospinal fluid ottorrhea or rinorrhea (a clear fluid running from the ears or nose), hemotympanum ( blood behind ear drum: the presence of blood in the tympanic cavity of the middle ear, diagnosed by otoscopy, presenting as partial or total occupancy of the tympanic membrane by a bright red to black-blue color depending on the duration of the blood in tympanic cavity).
Neurological examination:
Glascow coma scale (GSC)
Examination of the pupils: unequal pupils or a dilating pupil, usually indicate a focal mass lesion (such as an intracranial hematoma) and/or rising intracranial pressure.
Examination for the presence or absence of focal neurologic signs (focal neurologic signs, such as for example hemiparesis, speech disorder, diplopia, etc, should alert the physician to consider a significant injury and emergency CT and neurosurgical consultation).
The Glasgow Coma Scale (GCS) is used to evaluate the patient's level of consciousness: possible scores range from 3 (no response) to 15 (high response on all measures). The GCS evaluates three attributes: eye opening, verbal response, and best motor response (see below). When there is right/left or upper/lower asymmetry, use the best motor response to calculate the score. Despite the fact that drug and alcohol abuse is present in a significant number of trauma patients, it is preferrable to suspect that patients with a GCS score of less than 15 and an appropriate mechanism of trauma have a head injury, until proven otherwise. The GCS can be used to determine the severity of brain injury (minor injury GCS 13-15, moderate injury GCS 9 - 12, severe injury-coma GCS 3 - 8). This can also determine how urgently a CT scan must be obtained.
Here is a description of the Glasgow Coma Scale GCS:
Eye opening score
spontaneous 4
to voice 3
to painful stimuli 2
never 1
Verbal responce (speech) score
oriented 5
confused 4
inappropriate words 3
unintelligible sounds 2
none 1
Motor responce score
follows commands 6
localizes pain 5
withdrows from pain 4
flexor responce 3
extensor responce 2
none 1
Indications of a relatively high risk in a patient with head injury:
age >60
coagulation disorder, or patient on anticoagulation treatment
drug or alcohol intoxication
large swelling, or evidence of a skull fracture (these two characteristics are indicative of a strong force of injury)
GCS score <14
focal neurologic findings
blood glucose and basic biochemical tests ( urea, creatinine, sodium potassium, transaminases,etc)
blood typing
ECG
arterial blood gases (in cases of severe head trauma)
CT scan of the head without contrast
Examination for the presence or absence of focal neurologic signs (focal neurologic signs, such as for example hemiparesis, speech disorder, diplopia, etc, should alert the physician to consider a significant injury and emergency CT and neurosurgical consultation).
The Glasgow Coma Scale (GCS) is used to evaluate the patient's level of consciousness: possible scores range from 3 (no response) to 15 (high response on all measures). The GCS evaluates three attributes: eye opening, verbal response, and best motor response (see below). When there is right/left or upper/lower asymmetry, use the best motor response to calculate the score. Despite the fact that drug and alcohol abuse is present in a significant number of trauma patients, it is preferrable to suspect that patients with a GCS score of less than 15 and an appropriate mechanism of trauma have a head injury, until proven otherwise. The GCS can be used to determine the severity of brain injury (minor injury GCS 13-15, moderate injury GCS 9 - 12, severe injury-coma GCS 3 - 8). This can also determine how urgently a CT scan must be obtained.
Here is a description of the Glasgow Coma Scale GCS:
Eye opening score
spontaneous 4
to voice 3
to painful stimuli 2
never 1
Verbal responce (speech) score
oriented 5
confused 4
inappropriate words 3
unintelligible sounds 2
none 1
Motor responce score
follows commands 6
localizes pain 5
withdrows from pain 4
flexor responce 3
extensor responce 2
none 1
Indications of a relatively high risk in a patient with head injury:
age >60
coagulation disorder, or patient on anticoagulation treatment
drug or alcohol intoxication
large swelling, or evidence of a skull fracture (these two characteristics are indicative of a strong force of injury)
GCS score <14
focal neurologic findings
Usual diagnostic tests (work-up) for a patient with head trauma
complete blood count (CBC), coagulation testsblood glucose and basic biochemical tests ( urea, creatinine, sodium potassium, transaminases,etc)
blood typing
ECG
arterial blood gases (in cases of severe head trauma)
CT scan of the head without contrast
Treatment of traumatic brain injury
Secure the airway, check oxygen saturation and give supplemental oxygen if needed (see above). Cervical spine immobilization (full spinal immobilization in case of a severe head injury). Intubation if there is an indication (see above ).
Insert an intravenous cannula, infuse isotonic crystalloid solution if there is a low blood pressure (normal saline-N/S, or Ringer lactated R-L): If there is hypotension, guidelines recommend the use of small boluses (250ml) of isotonic crystalloid fluids to correct hypotension in case of severe brain trauma. Hypoxaemia, hypotension, hypercapnia and inadequate sedation (in an intubated patient) should all be corrected early.
Arrange for a noncontrast brain CT and neurosurgical consultation according to the estimated severity of head trauma ( in severe cases CT and neurosurgical consultation are needed promptly, without any waste of time). Note that on brain CT-scan foci of recent hemorrhage are depicted as hyperdence areas (almost white).
In severe brain injury with indications of increased intracranial pressure (ICP), ICP monitoring and the IV administration of mannitol and furosemide is indicated to reduce raised ICP.
Mannitol use prior to ICP monitoring is restricted to patients with signs of transtentorial herniation or progressive neurological deterioration. Mannitol is effective at doses of 0.25 g/kg to 1 g/kg body weight. Arterial hypotension (systolic blood pressure <90 mm Hg) should be avoided, when using mannitol.
Most patients with minor brain injury recover without any adverse events, but the physician should be cautious to detect early any decline in mental status, because approximately 3% of these patients have unexpected deterioration.
Indications for a brain CT scan in patients with minor brain injury
Age > 65 years.
GCS score <15 at 2 hours after injury. This is evidence suggesting persistent neurologic dysfunction
Indications suggestive of possible significant brain injury, such as loss of consciousness> 5 minutes, amnesia before impact >30 minutes, vomiting (more than two episodes).
Suspected open or depressed skull fracture or any sign of basilar skull fracture (see physical examination). A skull fracture usually indicates that the injury was caused by a strong force and so there is an increased possibility of underlying brain injury.
Dangerous mechanism of trauma (e.g., pedestrian struck by motor vehicle, person ejected from motor vehicle, fall from height more than 3 feet or five stairs).
the patient remains symptomatic or continues to have
neurologic abnormalities
there is moderate to severe headache
there is significant alcohol or drug intoxication
there are findings suggestive or diagnostic of a skull fracture
there are significant associated injuries
there is no reliable companion at home who could inform the emergency department in case a subsequent change in the patient's condition.
there are abnormalities on the CT scan
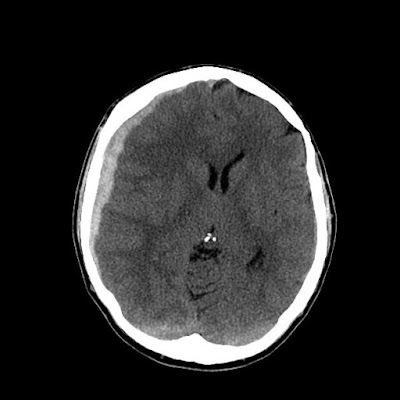
CT of a male patient 30 years old post head trauma with worsening headache . Is it normal ?
A skull fracture (disruption or break in bone continuity) may occur in the cranial vault or skull base. A skull fracture is generally the result of a significant amount of force transmitted to the head, thus it should increase the suspicion for possible intracranial injury.
There are several types of skull fractures : A closed fracture is covered by intact skin. An open, or compound, fracture is one with disrupted overlying skin. A stellate fracture has multiple lines radiating from a point. A linear fracture has a single line.
No specific treatment is usually required for closed skull fractures (with the exception of a fracture with depression greater than the cranial thickness, which will need a surgical operation). Open fractures are treated with debridement and repair of the scalp.
Indications for a surgical operation (craniotomy) in case of a skull fracture include depression greater than the cranial thickness, an intracranial hematoma, and involvement of the frontal sinus.
Mannitol use prior to ICP monitoring is restricted to patients with signs of transtentorial herniation or progressive neurological deterioration. Mannitol is effective at doses of 0.25 g/kg to 1 g/kg body weight. Arterial hypotension (systolic blood pressure <90 mm Hg) should be avoided, when using mannitol.
Minor traumatic brain injury
Definition: Minor traumatic brain injury is defined by a history of amnesia, disorientation, or transient loss of consciousness in a patient who is conscious and talking, with a GCS score 13 -15.Most patients with minor brain injury recover without any adverse events, but the physician should be cautious to detect early any decline in mental status, because approximately 3% of these patients have unexpected deterioration.
Indications for a brain CT scan in patients with minor brain injury
Age > 65 years.
GCS score <15 at 2 hours after injury. This is evidence suggesting persistent neurologic dysfunction
Indications suggestive of possible significant brain injury, such as loss of consciousness> 5 minutes, amnesia before impact >30 minutes, vomiting (more than two episodes).
Suspected open or depressed skull fracture or any sign of basilar skull fracture (see physical examination). A skull fracture usually indicates that the injury was caused by a strong force and so there is an increased possibility of underlying brain injury.
Dangerous mechanism of trauma (e.g., pedestrian struck by motor vehicle, person ejected from motor vehicle, fall from height more than 3 feet or five stairs).
Indications for hospital admission and neurosurgical consultation in a patient with minor brain trauma
For the definition of minor brain trauma please see above. The patient should be admitted to the hospital and a neurosurgeon should be consulted if :the patient remains symptomatic or continues to have
neurologic abnormalities
there is moderate to severe headache
there is significant alcohol or drug intoxication
there are findings suggestive or diagnostic of a skull fracture
there are significant associated injuries
there is no reliable companion at home who could inform the emergency department in case a subsequent change in the patient's condition.
there are abnormalities on the CT scan
When can the patient with minor traumatic head injury be discharged ?
If the patient is asymptomatic, fully awake and alert, and presents no neurologic abnormalities, then the patient may be observed for several hours, reexamined, and, if his or her condition reamains the same, safely discharged. For the patient to be discharged, the care of a companion who can observe the patient continually over the subsequent 24 hours is very useful. In all cases, written discharge instructions should be supplied recommending return to the emergency department if the patient develops headaches or manifests a decline in mental status or focal neurologic deficits.
CT of a male patient 30 years old post head trauma with worsening headache . Is it normal ?
ANSWER
There is a crescentic high density area on the right brain hemisphere. Brain hemorrhage is depicted on CT as a high denisty area. Here, findings are consistent with acute subarachnoid hemorrhage. The patient definitely needs a neurosurgical consultation. (Source: Radiopaedia org, a case by dr by Dr Yuri Shif https://radiopaedia.org/cases/subdural-haemorrhage-6 )
Some specific types of head injury
Skull fractures
A skull fracture (disruption or break in bone continuity) may occur in the cranial vault or skull base. A skull fracture is generally the result of a significant amount of force transmitted to the head, thus it should increase the suspicion for possible intracranial injury.
There are several types of skull fractures : A closed fracture is covered by intact skin. An open, or compound, fracture is one with disrupted overlying skin. A stellate fracture has multiple lines radiating from a point. A linear fracture has a single line.
No specific treatment is usually required for closed skull fractures (with the exception of a fracture with depression greater than the cranial thickness, which will need a surgical operation). Open fractures are treated with debridement and repair of the scalp.
Indications for a surgical operation (craniotomy) in case of a skull fracture include depression greater than the cranial thickness, an intracranial hematoma, and involvement of the frontal sinus.
Brain Concussion
A concussion is a temporary neurologic dysfunction following nonpenetrating head trauma. Symptoms resolve over minutes to hours and the head CT is normal, and deficits resolve over minutes to hours. Transient alteration of mental status (e g confusion or loss of consciousness, is usual. A very common feature is a memory difficulty, especially amnesia of the event.Cerebral contusion
Cerebral contusion is a hemorrhagic area in the brain with surrounding edema. A contusion of the brain can occur directly under the site of impact, or on the contralateral side (contrecoup lesion). Neurologic dysfunction is usually present and it can be profound and prolonged (impairment of consciousness such as confusion, or coma and focal neurologic deficits are also common). Occasionally subarachnoid hemorrhage is also present.Epidural hematoma
Epidural hematoma is a collection of blood between the skull and the dura matter. It is caused by injury of a meningeal artery usually from an overlying skull fracture. The classic clinical picture includes an initial transient loss of consciousness, followed by a lucid interval in which the patient is conscious with clear mentation and then there is gradual deterioration of the mental status. A late finding is a fixed and dilated pupil on the side of the lesion and hemiparesis on the other side. On CT scan it appears as a bright (white) area with a biconvex shape. It is the result of high pressure arterial bleeding and thus it can lead to brain herniation within hours of injury. Treatment requires prompt craniectomy for evacuation of the blood clot and hemostasis.An acute subdural hematoma (SDH)
An acute subdural hematoma (SDH) is an accumulation of blood between the arachnoid membrane and the dura, resulting from venous bleeding, usually from a bridging vein running from the cerebral cortex to the dural sinuses. People with brain atrophy, such as elderly and alcoholic patients are at higher risk for subdural hematoma formation after head trauma.On head CT scan, the hematoma is bright or mixed-density and crescent-shaped.
Indications for surgical operation (open craniotomy) for evacuation of acute SDH are the following: thickness >1 cm, or midline shift >5 mm, or GCS drop by ≥ 2 points from the time of injury.
A hematoma managed without an operation may stabilize and eventually reabsorb, or evolve into a chronic SDH. The prognosis for functional recovery is significantly worse for acute subdural hematoma than for epidural hematoma because the former is associated with greater primary injury to the brain parenchyma.
Prompt recognition of an acute SDH and intervention minimizes secondary injury of the brain and improves neurologic recovery.
A video I strongly recommend this video, about brain trauma (diagnosis and management) LINK:
https://www.youtube.com/watch?v=aIXghKWhegA
GO BACK TO THE TABLE OF CONTENTS
LINK: Emergency medicine book-Table of contents
Prompt recognition of an acute SDH and intervention minimizes secondary injury of the brain and improves neurologic recovery.
A video I strongly recommend this video, about brain trauma (diagnosis and management) LINK:
https://www.youtube.com/watch?v=aIXghKWhegA
GO BACK TO THE TABLE OF CONTENTS
LINK: Emergency medicine book-Table of contents
Bibliography and Links
Dinsmore J. Traumatic brain injury: an evidence-based review of management. Contin Educ Anaesth Crit Care Pain 2013; 13: 189-195. doi: 10.1093/bjaceaccp/mkt010
LINK
Traumatic brain injury: an evidence-based review of management
Best-evidence Review of Acute Care for Moderate to Severe Traumatic Brain Injury Reviewer Mark Ayson MBChB DPH- Date Report Completed August 2011
A Book :
National Collaborating Centre for Acute Care Head Injury Triage, assessment, investigation and early management of head injury in infants, children and adults. The Royal College of Surgeons of England 2007.
LINK
Traumatic brain injury: an evidence-based review of management
Best-evidence Review of Acute Care for Moderate to Severe Traumatic Brain Injury Reviewer Mark Ayson MBChB DPH- Date Report Completed August 2011
A Book :
National Collaborating Centre for Acute Care Head Injury Triage, assessment, investigation and early management of head injury in infants, children and adults. The Royal College of Surgeons of England 2007.
LINK
https://www.ncbi.nlm.nih.gov/books/NBK53036/pdf/Bookshelf_NBK53036.pdf
Marik PE, Varon J, Trask T. Management of Head Trauma. Chest 2002;122;699-711
LINK
https://www.med.illinois.edu/depts_programs/sciences/clinical/internal_med/residency/curriculum/Critical%20Care%20Literature/CNS/Head%20Trauma.pdf
Marik PE, Varon J, Trask T. Management of Head Trauma. Chest 2002;122;699-711
LINK
https://www.med.illinois.edu/depts_programs/sciences/clinical/internal_med/residency/curriculum/Critical%20Care%20Literature/CNS/Head%20Trauma.pdf
No comments:
Post a Comment